Based on: Baseline Cardiac Biomarker Levels as Predictors of Cancer Risk in the MESA Cohort
By Iqra Sharjeel

Cardiovascular disease (CVD) and cancer are the two leading causes of death globally. While they have traditionally been studied separately, research over the past decade has increasingly pointed to shared biological pathways, such as inflammation, oxidative stress, and cellular remodeling. Many of the same risk factors—such as age, obesity, smoking, sedentary lifestyle, and diabetes—contribute to both diseases.
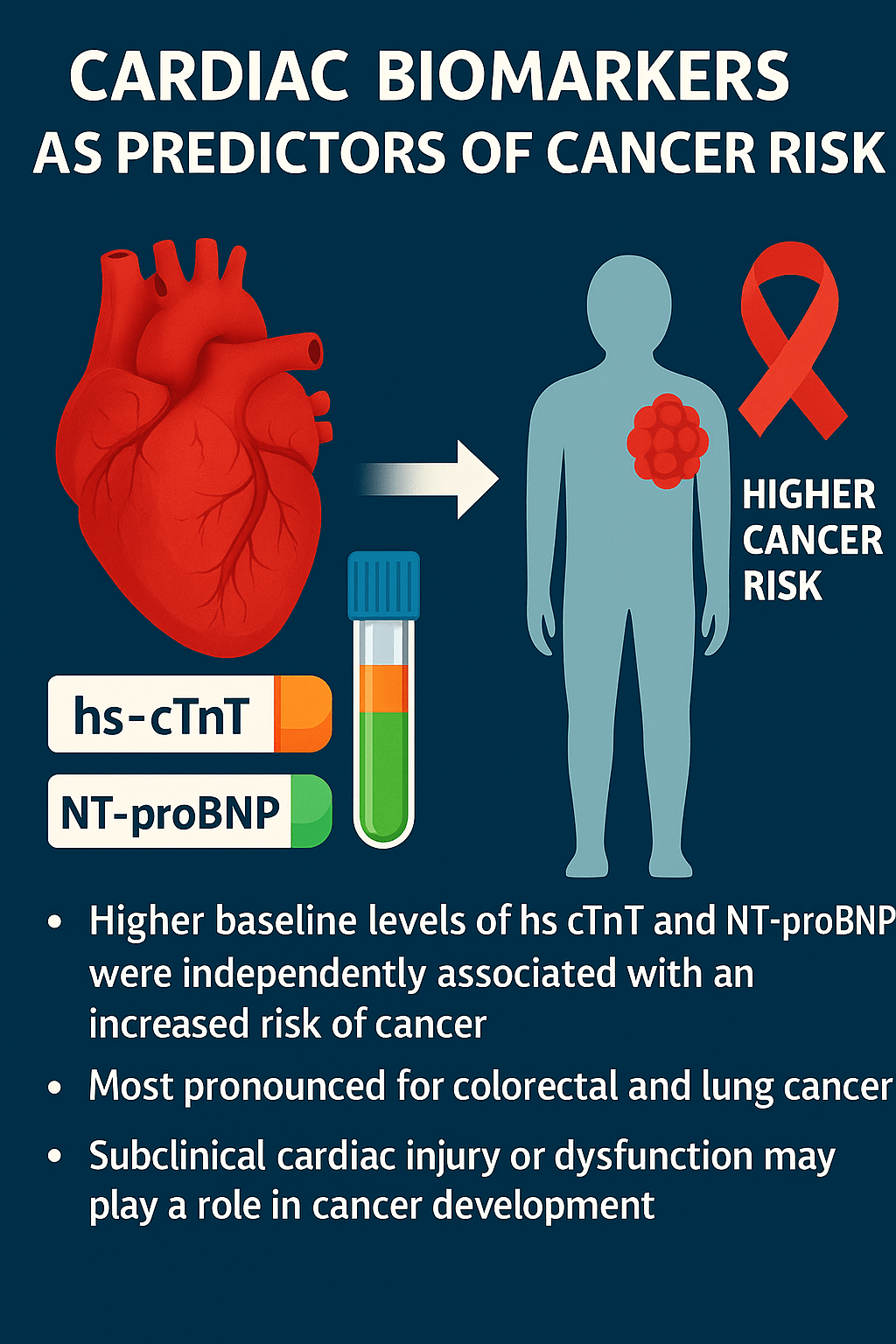
Cardiac biomarkers like high-sensitivity cardiac troponin T (hs-cTnT) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) are used to detect subclinical myocardial injury and stress, even in the absence of overt heart failure. These markers are well-established for cardiac risk prediction—but can they also predict future cancer development, even in individuals without known cardiovascular or oncologic conditions?
Study Objective
To determine whether baseline levels of hs-cTnT and NT-proBNP are associated with long-term cancer risk in participants of the MESA study—specifically those who were free of clinical cardiovascular disease and cancer at baseline. The study also explored whether race/ethnicity and sex influenced these associations.
Study Design and Population
- Study type: Prospective, longitudinal cohort study
- Cohort: Multi-Ethnic Study of Atherosclerosis (MESA)
- Participants: 6,244 adults aged 45–84 years (52.7% female)
- Exclusion at baseline: No self-reported cancer or clinical CVD
- Follow-up duration: Median 17.8 years
- Ethnic diversity: Non-Hispanic White, Black, Hispanic/Latino, and Chinese Americans across 6 U.S. field centers
Biomarker Measurement
- hs-cTnT and NT-proBNP were measured in blood samples at baseline.
- Participants were categorized into groups:
- hs-cTnT: 5 groups based on ranges (e.g., <3 ng/L to ≥8.8 ng/L)
- NT-proBNP: Quartiles
- Levels were also log-transformed and standardized for statistical modeling.
Methods of Analysis
- Cancer incidence was identified via hospitalization records using ICD-9 codes (excluding non-melanoma skin cancers).
- Statistical method: Cox proportional hazards models
- Two types of adjustments were made:
- Minimally adjusted models: Controlled for demographics (age, sex, race/ethnicity), BMI, insurance, and education.
- Fully adjusted models: Included lifestyle and clinical factors (smoking, blood pressure, cholesterol, diabetes, kidney function, physical activity, and diet).
Key Findings
Overall Cancer Risk:
- 820 participants developed cancer over 17.8 years.
- All-cancer incidence rate: 91.2 cases per 10,000 person-years.
- Participants with higher baseline biomarker levels had a significantly higher risk of developing cancer.
hs-cTnT:
- Fully adjusted hazard ratio (HR) for all cancers: 1.18 (95% CI: 1.09–1.27, P < 0.001)
NT-proBNP:
- Fully adjusted HR for all cancers: 2.41 (95% CI: 1.30–4.49, P = 0.006)
Site-Specific Cancer Associations
| Cancer Type | hs-cTnT Association | NT-proBNP Association |
| Colorectal | HR: 1.39 (significant) | HR: 1.66 (significant) |
| Lung | Not significant | HR: 1.31 (significant) |
| Breast/Female-specific | Not significant | Not significant |
| Prostate | Not significant | Trend observed but not significant after full adjustment |
Race, Sex, and Age Differences
- No statistically significant interactions between biomarker levels and sex or age were observed.
- A small interaction with race/ethnicity was detected for breast and female-specific cancers and hs-cTnT, but no individual racial subgroup had a clear significant effect.
- This suggests findings are broadly applicable across ethnic groups and both sexes.
Interpretation and Biological Insight
The findings support the theory that subclinical cardiac dysfunction or injury—indicated by elevated hs-cTnT and NT-proBNP—may precede or promote cancer development, possibly through:
- Chronic inflammation
- Fibrotic tissue remodeling
- Circulating stress signals from heart to other organs
- Activation of immune responses
The association with colorectal cancer is particularly intriguing, as cardiac troponin T (TNNT2) has been detected in colorectal tumors and may promote tumor progression. Similarly, NT-proBNP may be elevated in lung cancer patients even without heart failure, possibly linked to stress responses in pulmonary disease.
Limitations
- Cancer diagnoses based on hospitalization codes—outpatient and undiagnosed cases could be missed.
- Detection bias may occur if elevated biomarkers led to more frequent healthcare encounters.
- Cancer subtypes (like sex-specific cancers) had relatively few cases, limiting power.
- Lack of adjudicated cancer data, staging, or treatment details.
- No correction for multiple testing—caution needed when interpreting marginal associations.
- Participants were generally healthier than the broader population.
Conclusion
In this large, multiethnic cohort free of clinical CVD and cancer at baseline, elevated levels of hs-cTnT and NT-proBNP were independently associated with a significantly higher risk of future cancer, particularly colorectal and lung cancers. These findings expand the predictive value of cardiac biomarkers beyond CVD and suggest their potential use in oncologic risk stratification.
Clinical Perspective
- Medical Knowledge: hs-cTnT and NT-proBNP can be early warning signals not only for heart disease but also for certain cancers.
- Translational Outlook: Incorporating cardiac biomarkers into cancer screening protocols may help identify at-risk individuals years before diagnosis, especially for cancers like colorectal.







You must be logged in to post a comment.